A new choice in the local treatment of articular tuberculosis
Una nueva opción en el tratamiento local de la tuberculosis articular
Uma nova opção no tratamento da tuberculose articular
A new choice in the local treatment of articular tuberculosis
José María Hernández-Mateo1
José Antonio Matas-Díaz1
Francisco Javier Vaquero-Martín1, 2
Pablo Sanz-Ruiz1, 2
1 Department of Orthopaedic Surgery. General University Hospital Gregorio Marañón, Madrid, 28007, Spain. 2 Complutense University of Madrid, Madrid, 28040, Spain.
Correspondence to:
José María Hernández-Mateo
E-mail: josehermat@gmail.com
Abstract.
OBJECTIVES: The aim of this case series is to introduce a new choice in local treatment of tuberculosis arthritis. In this study, we used sulfate calcium beads mixed with isoniazid and rifampicin, that allows to carry antibiotics to the site of infection.
METHODS: Between January 2017 and December 2020, we performed 5 cases of surgical treatment in two stages of knee tuberculous infection: 4 in total knee arthroplasty and one of them, in a native knee. Mean age was 72 ± 14 years (range 47-87 years), one were male and five was females.. Mean follow-up was 37 months (range 19-59 months). One patient had concomitant infection with S. epidermis. All cultures obtained after the first and the second stage were negative after prolonged incubation, as was the molecular biology study.
At first stage, it was decided to carry out mobile antibiotic-impregnated cement spacers adding streptomycin and vancomycin. In all cases, time interval between first and second stage was less than three months. At second stage, it was decided to carry out a rotating-hinge revision total knee arthroplasty.
RESULTS: Mean preoperative ROM was 79° ± 39.1° (range 10°-100°) and the postoperative ROM was 104° ± 11.4° (range 90°-120°). There were no significant differences in Knee Society Score and SF-12 scores before 6 weeks and 6 months after surgery. There have been no soft tissue complications. No post-surgical seroma or persistent surgical drainage was observed in any of the cases. We did not report any cases of hypercalcaemia. In none of the cases we were able to observe heterotopic calcifications, neither in radiological imaging nor intraoperatively. During follow-up, we did not observe radiologic or clinic signs of loosening. No patient required further surgery. The mean time between stages was 10 ± 1 weeks (range 9-11 weeks).
CONCLUSIONS: Sulfate calcium beads may be effective to carry specific antibiotics to infection site when these drugs are not available to blend it with cements.
Level of evidence: IV. Case series study.
Keywords: Periprosthetic infection, Tuberculosis arthritis, Calcium sulfate beads
RESUMEN
OBJETIVOS: El objetivo de esta serie de casos es presentar una nueva opción en el tratamiento local de la artritis tuberculosa. En este estudio, utilizamos perlas de sulfato de calcio mezcladas con isoniazida y rifampicina, que permiten llevar los antibióticos al sitio de la infección.
MÉTODOS: Entre enero de 2017 y diciembre de 2020 realizamos 5 casos de tratamiento quirúrgico en dos estadios de infección tuberculosa de rodilla: 4 en artroplastia total de rodilla y uno de ellos, en rodilla nativa. La edad media fue de 72 ± 14 años (rango 47-87 años), uno era hombre y cinco mujeres. El seguimiento medio fue de 37 meses (rango 19-59 meses). Un paciente tenía una infección concomitante con S. epidermis. Todos los cultivos obtenidos tras la primera y segunda etapa fueron negativos tras una incubación prolongada, al igual que el estudio de biología molecular.
En una primera etapa se colocaron espaciadores móviles de cemento impregnados de estreptomicina y vancomicina. En todos los casos, el intervalo de tiempo entre la primera y la segunda etapa fue inferior a tres meses. En una segunda etapa, se decidió realizar una artroplastia total de rodilla de revisión en bisagra rotatoria.
RESULTADOS: El ROM preoperatorio medio fue de 79 ± 39,1° (rango 10°-100°) y el ROM postoperatorio fue de 104° ± 11,4° (rango 90°-120°). No hubo diferencias significativas en las puntuaciones de la Sociedad de la Rodilla y SF-12 antes de las 6 semanas y 6 meses después de la cirugía. No ha habido complicaciones de tejidos blandos. No se observó seroma posquirúrgico ni drenaje quirúrgico persistente en ninguno de los casos. No reportamos ningún caso de hipercalcemia. En ninguno de los casos pudimos observar calcificaciones heterotópicas, ni en la imagen radiográfica ni intraoperatoriamente. Durante el seguimiento no observamos signos radiográficos ni clínicos de aflojamiento. Ningún paciente requirió cirugía adicional. El tiempo medio entre estadios fue de 10 ± 1 semana (rango 9-11 semanas).
CONCLUSIONES: Las perlas de sulfato de calcio pueden ser efectivas para llevar antibióticos específicos al sitio de la infección cuando estos medicamentos no están disponibles para mezclarlos con los cementos.
Nivel de evidencia: IV. Estudio de serie de casos.
Palabras clave: Infección periprotésica, Artritis tuberculosa, Perlas de sulfato de calcio
Introduction.
General treatment of osteoarticular infections is based on two fundamental pillars: radical surgical debridement and adequate antibiotic treatment. Unfortunately, many of the available antibiotics have shown insufficient penetration and bioavailability in the osteoarticular territory. In recent years, there is a growing interest in local administration of antibiotics to achieve high concentrations in situ, which could be effective in an adverse medium such as biofilm, avoiding the toxic effects that would exist if such concentrations were achieved with systemic administration. Of all the local antibiotic delivery options, the use of bone cement loaded with different antibiotics (ALBC) has been the most widely mechanism [1].
In the specific case of septic arthritis secondary to tuberculous etiology, there is currently no consensus on the type of surgical treatment to be applied. Historically synovectomy, resection arthroplasty, arthrodesis or amputation have been considered, with unsatisfactory results. In the case of the last three, these techniques are useful for healing the infection, but they severely limit the functionality of the affected limb [2] [1] [3]. In the case of replacement arthroplasty, it is mandatory to have ensured resolution of the active infection prior to implantation, and an extended time interval is necessary for the patient to receive systemic anti-tuberculosis treatment [3]. Currently, some series have shown good results with short intervals, although these are reduced to isolated cases, and there is still no clear evidence on this [4-6].
The combination of local antibiotic therapy with surgical debridement is an interesting option to reduce the time between surgeries and increase the rate of surgical success. However, the complexity of antibiotic treatment of mycobacterial infections, where treatment with at least four drugs is necessary, along with the impossibility of using some of them in PMMA because they interact with its polymerisation process (such as isoniazid and rifampicin) [7] has limited their potential use in local therapy.
The use of calcium sulphate beads as a means of transportation of local antibiotic has shown to be extremely useful, as demonstrated by the exponential increase in the number of authors recommending their use [8-10]. Among their theoretical advantages, undoubtedly one of the most attractive is that these beads do not require removal, as they are reabsorbed in no more than 3 months. In addition, they have a predictable supratherapeutic elution profile, eluting all the antibiotic added and allowing many different antibiotics to be mixed, including some that are not possible to add to bone cement [11][12].
The aim of this manuscript is to present a new simple, safe, and reproducible surgical protocol for the treatment of tuberculous joint infection, especially in the context of periprosthetic infections, based on the use of local antibiotherapy using calcium sulphate beads as a vehicle to achieve high local concentrations of antituberculous drugs in patients with Mycobacterium tuberculosis arthritis.
Material and methods.
All patients gave their verbal informed consent before being included in this study. This was a retrospective case series and data was collected and performed in accordance with the principles of the 1964 Declaration of Helsinki as revised in 2013.
Between January 2017 and December 2020, 5 consecutive cases of knee tuberculosis infection (two in primary arthroplasty, two in revision arthroplasty and one in native knee) were treated with a new surgical protocol. The definition of infection was based on the modified Musculoskeletal Infection Society criteria, recommended at the 2013 International Consensus Meeting. All patients underwent two-stage surgery with implantation of a hinged spacer between the first and second surgeries along with the use of calcium sulphate beads with anti-tuberculoses drugs, allowing for maintenance of knee mobility between surgeries. The medical records of all patients were reviewed to obtain clinical and microbiological data, details of the initial prosthesis implantation, as well as previous surgeries, antibiotic therapy used (with special attention to anti-tuberculosis therapy and its duration) and follow-up results. Data recorded included patient demographics, surgical indications, number of previous surgeries, surgical complications, other microbiological organisms identified, antibiotic therapy, and subsequent follow-up results. Patient comorbidities were recorded using the American Society of Anesthesiologists (ASA) score and the Charlson comorbidity index score. Clinical assessment of each patient included the Oxford Knee Score (OKS) and the 12-item short form health survey (SF-12) assessed preoperatively at 6 weeks and 6 months after surgery, and at annual follow-up visits.
Surgical technique.
With the patient in the supine position and under regional anesthesia, an anterior approach to the knee is performed using conventional medial patellofemoral arthrotomy. Once the joint is approached, an exhaustive debridement of the femoral drippings and prepatellar recess is performed until adequate exposure is achieved. If adequate exposure was not achieved, tibial crest osteotomy was performed. After completion of debridement, the previous implant was removed if present. Multiple protocoled samples for culture are taken during this step from the diaphysis, distal femur and proximal tibia. We completed a radical debridement of any devitalized or fibrotic tissue, washing with 9 liters of saline liquid plus pure betadine and hydrogen peroxide and start building the cement spacer.
In all cases, 3 pre-filled cement packs with 1g gentamicin and 1g clindamycin (Copal G+C, Heraeus Medical GmbH, Wehrheim, Germany) were used, two for the femoral shield and one for the tibial plate, to which 2g streptomycin powder + 2g vancomycin were added for each cement pack used. Once the articulating spacer was implanted, after checking adequate stability and range of motion, 30 cc of calcium sulphate beads (STIMULAN® - Biocomposites® - Keele, UK) pre-loaded with antibiotic were added, following the usual surgical technique. 9 Two 10cc packets containing 400mg rifampicin powder and 300mg liquid isoniazid and one 10cc packet containing 2g streptomycin were used. The beads were inserted around both the femur and tibia, avoiding placement between the two components of the spacer. Finally, a plane closure was performed, paying special attention to the tightness of the arthrotomy closure in order to minimize the risk of prolonged drainage, previously observed with the intra-articular use of calcium sulphate [13]. (Figure 1) (Figure 2).

Figure 1
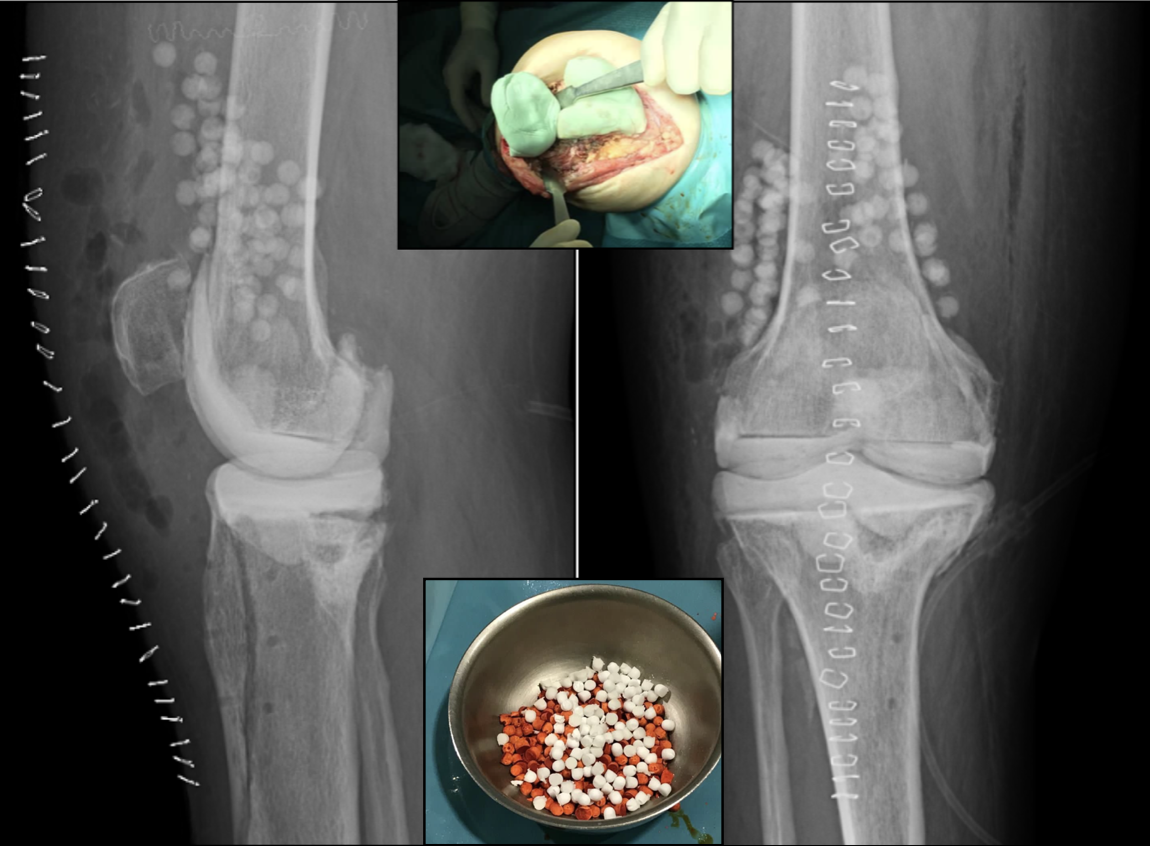
Figure 2
Mobilisation and partial weight bearing were allowed from the first postoperative day, both spontaneously and with the aid of an arthromotor. Until the results of the cultures and panbacterial CRP were obtained, the patients remained on empirical antibiotherapy with teicoplanin 600mg/12h IV and meropenem 1g/24h IV according to our centre's protocol, in addition to targeted antituberculosis therapy. Once the absence of other microorganisms was confirmed, only antituberculosis treatment was maintained.
After confirming the resolution of the infection by normalisation of serological parameters, the second surgical stage was performed by implanting a revision hinge-type total knee prosthesis (Endo-Model®; Waldemar Link® - Hamburg, Germany), maintaining the same antibiotic therapy as in the first stage until negative cultures and CRP were confirmed in the second stage.
Results.
Five patients with tuberculous knee infection were treated with this protocol, of which one were male (20%) and four was females. Mean standard deviation age was 72 ± 14 years (range 47-87 years). Mean SD follow-up was 37 ± 17 months (range 19-59 months). Four patients had periprosthetic tuberculous infection, and one patient on native knee. None of the patients were smokers or chronic users of corticosteroids. None of the patients had a previous history of cancer, nor had they received immunosuppressive treatment.
Microbiological confirmation was obtained in all cases prior to surgical treatment, in the samples obtained in the first stage. One patient had concomitant infection with S. epidermis (20%). All cultures obtained in the second stage were negative after prolonged incubation, as was the molecular biology study.
The range of motion (ROM) of each patient is shown in Table 1, with the mean preoperative ROM being 79° ± 39.1° (range 10°-100°) and the postoperative ROM being 104° ± 11.4° (range 90°-120°). There were no significant differences in Knee Society Score and SF-12 scores before 6 weeks and 6 months after surgery. There were also no differences in subsequent annual clinical follow-ups.
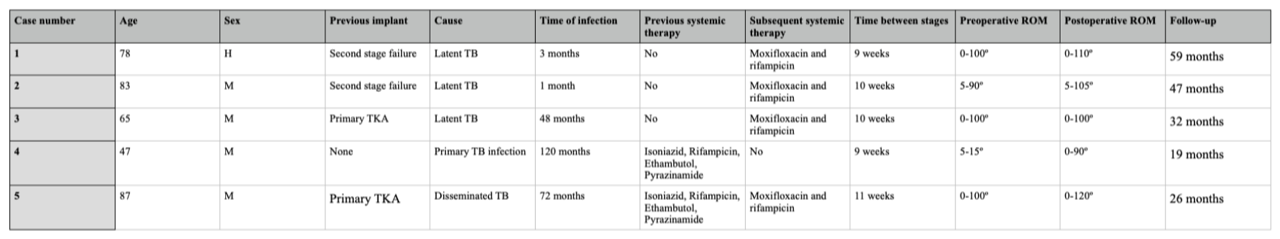
Table 1
There have been no soft tissue complications because of the use of these calcium sulphate beads. No post-surgical seroma or persistent surgical drainage was observed in any of the cases. We did not report any cases of hypercalcaemia after bead implantation. In none of the cases we were able to observe heterotopic calcifications, neither in radiological imaging nor intraoperatively [9-13]. During follow-up, we did not observe increased radiolucency or other signs of loosening. No patient required further surgery.
Three of the patients did not receive previous systemic anti-tuberculosis treatment, being a latent form of tuberculosis. The other two cases received polytherapy with 4 drugs for 2 months and 1 year, respectively. The mean time between stages was 9.8 ± 0.8 weeks (range 9-11 weeks). Four patients received post-surgical systemic treatment for 6 weeks with moxifloxacin and rifampicin.
Discussion.
Septic arthritis of tuberculous etiology is experiencing an increase in its incidence in occidental countries because of the continuous migratory flow, as well as the increase of immunosuppressed patients (due to HIV, immunosuppressive therapies for rheumatological diseases or cancer) [14][15]. Parallel to this increase in tuberculous arthritis, cases of periprosthetic mycobacterial infections have been observed, although now they are limited to isolated cases [16-19].
Regarding the surgical techniques that can be used in the treatment of tuberculous infection in the native knee, arthrodesis has been the most widely used in recent decades, due to the great existing joint destruction and the difficulty in ensuring healing of the tuberculous bone infection, which would contraindicate the implantation of a prosthesis. However, total knee arthroplasty provides better functional results than arthrodesis, with the latter currently relegated to being the last limb-salvage technique [3][5].
There is a controversy about how long we should wait to perform total knee arthroplasty after tuberculous arthritis or after periprosthetic infection. Classically, it was postulated to wait from more than 1 year (up to 30) before surgery could be performed [14][15]. More recent publications have performed arthroplasty in active infections with prior systemic treatment for several weeks, with good results, always assuming the risk of reactivation [4][5]. Sultan et al. conclude in a systematic review that a two-stage exchange should be performed in patients in whom tuberculosis infection has been diagnosed and treated for more than 1 year. In addition, patients should receive postoperative systemic antituberculous treatment for at least 3 weeks [3]. However, there are reports that only recommend performing a two-stage primary arthroplasty in patients in whom CRP and ESR remain elevated after several months of systemic treatment [4][5][20].
In the specific case of periprosthetic infections, two-stage replacement currently seems to be more suitable for complex germs to treat, so it makes sense to approach M. tuberculosis infection in this way, as it is an intracellular pathogen with a great capacity for the formation of intraosseous caverns with latent forms of the disease inside [14]. In all published series the spacer used was fixed [3]. The use of a hinged cement spacer could allow an adequate preoperative joint balance to be maintained before the second stage.
Comparing our postoperative ROM results after 2-stage surgery, we achieved similar results to the study by Zeng et al. [20]. In the case series published by Ozturkmen et al. [5] and Han et al. [21] no results on postoperative joint balance were published.
There are multiple series that support the existence of a higher success rate in controlling periprosthetic infection when antibiotherapy is used locally [16]. In the specific case of tuberculous septic arthritis, infection control failure rates vary after arthroplasty, and can be as high as 33% [3-5][20]. Poor prognostic factors include no previous anti-tuberculosis treatment or chronic administration of corticosteroids [3].
Local administration of appropriate antituberculous drugs may increase their joint concentration several times more than the systemic route and decrease the rate of persistence of infection. Direct local administration of drugs such as streptomycin by washing after debridement has not been shown to be useful [4][20]. However, some authors have obtained encouraging results in the treatment of tuberculous arthritis sequelae by adding streptomycin to PMMA [4][5][16][22]. Unfortunately, there are no reports of its usefulness in the treatment of prosthetic infections, as other tuberculostatics cannot be applied to bone cement because they affect the polymerisation capacity of PMMA (rifampicin [21] and isoniazid [7]) or have particularly low elution rates (isoniazid [1]).
PMMA beads and calcium sulphate-based vehicles for antibiotic transport have been postulated as a local adjuvant treatment. Calcium sulphate beads are an effective alternative for compounds that cannot be added to cement. They can release 100% of their antibiotic load for weeks, providing concentrations several times higher than the minimum inhibitory concentration (MIC) to eliminate each pathogen. This ensures a safe systemic toxicity profile [9][12]. The fact that they are resorbable ensures that there is no foreign body susceptible to colonization after antibiotic release is complete [8][9].
In our study, we reported a concomitant infection, with other reports showing up to 45% of concomitant infections, most frequently of the genus Staphylococcus. The use of a PMMA spacer preloaded with gentamicin, clindamycin and vancomycin increases the elution of streptomycin and protects us from the presence of most of the usual microorganisms and protects the spacer from possible colonization by other pathogens [16].
This study is subject to certain limitations. Firstly, the small number of patients presented. Nevertheless, most published series of mycobacterial periprosthetic infections are limited to only a few cases. Secondly, there is no control group. However, in our experience based on the treatment of periprosthetic infections, the use of calcium sulphate beads together with ALBC articulating spacers is a safe technique that allows us to achieve the highest success rate, making it difficult to develop a control group without it. Thirdly, follow-up is short, and we still do not know the results after 3 years, which is especially important in infections by microorganisms with extensive silent activity such as mycobacteria. Even so, the follow-up of our series is longer than the accepted follow-up to affirm the cure of a periprosthetic infection.
In our opinion, this article constitutes the first report in the literature of treatment of joint tuberculosis using a hinged cement spacer in conjunction with the use of calcium sulphate beads with added antituberculous as a means of local release of multiple antibiotics.
This case series aims to demonstrate a new surgical protocol for treating tuberculous knee infections, both periprosthetic and in the native knee. The use of calcium sulphate beads is a useful resource for transporting antibiotics to the site of infection in compounds that are not suitable for mixing with cement.
References.
1. Bridgens J, Davies S, Tilley L, Norman P, Stockley I. Orthopaedic bone cement: do we know what we are using? J Bone Joint Surg Br. 2008; 90-B:643–7.
2. Bae DK, Yoon, Kim HS, Song SJ. Total knee arthroplasty in stiff knees after previous infection. J Bone Joint Surg Br, 2005. 87-B:333–6.
3. Sultan A, Cantrell W, Rose E, Surace P, Samuel L, Chughtai M, et al. Total knee arthroplasty in the face of a previous tuberculosis infection of the knee: what do we know in 2018? Expert Rev Med Devices. 2018; 15:717-24.
4. Habaxi KK, Wang L, Miao XG, Alimasi W, Zhao X, Su J, Yuan H. Total knee arthroplasty treatment of active tuberculosis of the knee: a review of 10 cases. Eur Rev Med Pharmacol Sci. 2014; 18:3587-92.
5. Öztürkmen Y, Üzümcügil O, Karamehmetoglu M, Leblebici C, Caniklioglu M. Total knee arthroplasty for the management of joint destruction in tuberculous arthritis. Knee Surg Sports Traumatol Arthrosc. 2014; 22:1076-83.
6. Shembekar A, Babhulkar S. Chemotherapy for osteoarticular tuberculosis. Clin Orthop Relat Res. 2002. 398:20–26.
7. Leclere L, Sechriest F, Holley K, Tsukayama D. Tuberculous Arthritis of the Knee Treated with Two-Stage Total Knee Arthroplasty. A Case Report. J Bone Joint Surg Am. 2009; 91-A:186-91.
8. McConoughey S, Howlin R, Wiseman J, Stoodley P, Calhoun J. Comparing PMMA and calcium sulfate as carriers for the local delivery of antibiotics to infected surgical sites. J Biomed Mater Res B Appl Biomater. 2015; 103:870-7.
9. McPherson EJ, Dipane MV, Sherif SM. Dissolvable antibiotic beads in treatment of preiprosthetic joint infection – the use of synthetic pure calcium sulfate (Stimulan®) impregnated with vancomycin and tobramycin. Reconstr Rev. 2013:32.
10. Risitano S, Sabatini L, Atzori F, Massè A, Indelli P. Static antibiotic spacers augmented by calcium sulphate impregnated beads in revision TKA: Surgical technique and review of literature. J Orthop. 2018; 15:313-8.
11. Abosala A, Ali M. The Use of Calcium Sulphate beads in Periprosthetic Joint Infection, a systematic review. J Bone Jt Infect. 2020; 5:43-9.
12. Wahl P, Guidi M, Benninger E, Rönn K, Gautier E, Buclin T, et al. The levels of vancomycin in the blood and the wound after the local treatment of bone and soft-tissue infection with antibiotic-loaded calcium sulphate as carrier material. Bone Joint J. 2017; 99-B:1537-44.
13. Lee G, Khoury J, Bell J-E, Buckwalter J. Adverse reactions to OsteoSet bone graft substitute, the incidence in a consecutive series. Iowa Orthop J. 2002; 22:35-8.
14. Tuli SM. General principles of osteoarticular tuberculosis. Clin Orthop Relat Res, 2002. 398:11–9.
15. Watts HG, Lifeso RM. Tuberculosis of bones and joints. J Bone Joint Surg Am, 1996. 78-A:288–99.
16. Chang CH, Hu CC, Chang Y, Hsieh pH, Shig HN, Ueng S. Two-stage revision arthroplasty for Mycobacterium Tuberculosis periprosthetic joint infection: An outcome analysis. PLoS ONE. 2018; 13:e0203585.
17. Kim S, Kim J. Late onset Mycobacterium tuberculosis infection after total knee arthroplasty: a systematic review and pooled analysis. Scand J Infect Dis. 2013; 45:907-14.
18. Lee CL, Wei YS, Ho YJ, Lee CH. Postoperative Mycobacterium tuberculosis infection after total knee arthroplasty. Knee. 2009; 16:87-9.
19. Marmor M, Parnes N, Dekel S. Tuberculosis infection complicating total knee arthroplasty: report of 3 cases and review of the literature. J Arthroplasty. 2004; 19:397-400.
20. Zeng M, Xie J, Wang L, Hu Y. Total knee arthroplasty in advanced tuberculous arthritis of the knee. Int Orthop. 2016; 40:1433-9.
21. Han CD, Oh T, Cho SN, Yang JH, Park KK. Isoniazid Could Be Used for Antibiotic-loaded Bone Cement for Musculoskeletal Tuberculosis: An In Vitro Study. Clin Orthop Relat Res. 2013 Jul;471(7):2400-6. https://doi.org/10.1007/s11999-013-2899-5.
22. Masri BA, Duncan CP, Jewesson P, Ngui-Yen J, Smith J. Streptomycin-loaded bone cement in the treatment of tuberculous osteomyelitis: an adjunct to conventional therapy. Can J Surg. 1995; 38:64–8.
23. Kallala R, Edwin Harris W, Ibrahim M, Dipane M, McPherson E. Use of Stimulan absorbable calcium sulphate beads in revision lower limb arthroplasty: Safety profile and complication rates. Bone Joint Res. 2018; 7:570-9.
24. Dobbs T, Webb R. Chemotherapy of Tuberculosis. Microbiol Spectr. 2017; 5.
25. Mittal Y, Fehring T, Hanssen A, Marculescu C, Odum S, Osmon D. Two-stage reimplantation for periprosthetic knee infection involving resistant organisms. J Bone Joint Surg Am. 2007; 89-A:1227-31.
Figures
Figure 1: Calcium sulphate beads, already mixed with rifampicin (orange) and isoniazid (white).
Figure 2: Copal C+G® articulated spacer, with added vancomycin and streptomycin.
